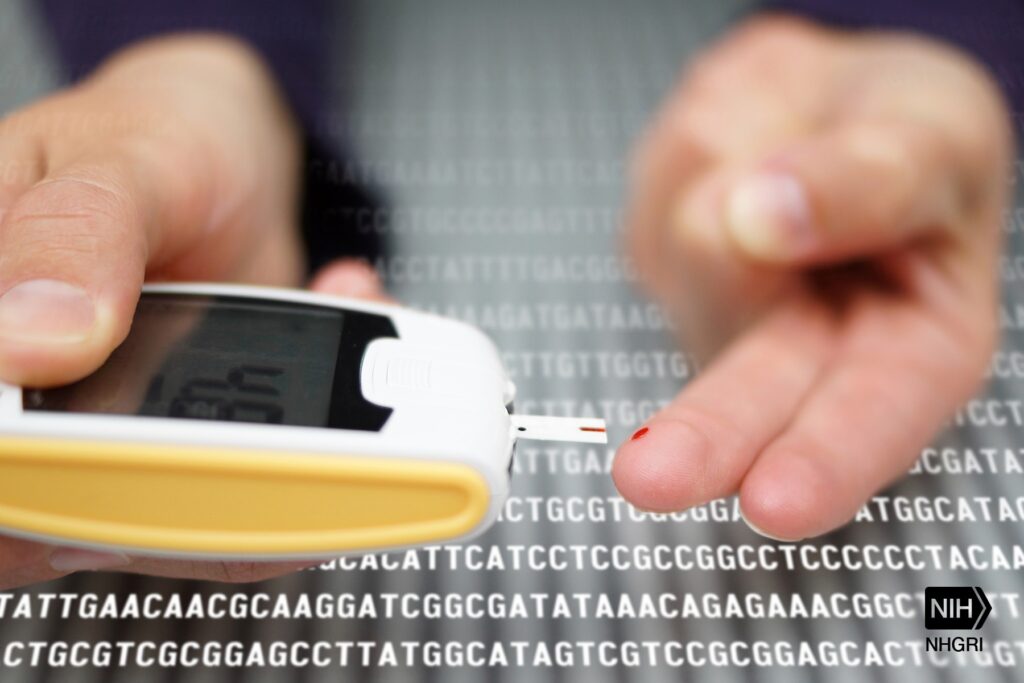
Managing type 1 diabetes just shed one of its most dangerous requirements. A 42-year-old Swedish man received the world’s first transplant of gene-edited insulin-producing cells that survived in his body for months without any anti-rejection medication—a breakthrough that could reshape how you think about diabetes treatment.
This isn’t another “cure in 10 years” promise that’s circulated since MySpace was relevant. In December 2024, researchers successfully used CRISPR technology to modify donor islet cells, removing the molecular targets that typically trigger your immune system’s attack response while adding proteins that essentially tell your body “don’t destroy these.”
The Technical Breakthrough That Changes Everything
This gene-editing approach eliminates the deadliest aspect of traditional islet transplants.
The procedure involved 17 carefully planned injections of genetically modified islet cells—the pancreatic workhorses responsible for insulin production. Here’s what made these cells different:
- HLA-I and HLA-II antigens completely removed – eliminating the primary immune system triggers that destroy transplanted tissue
- Extra CD47 protein added – a molecular “don’t eat me” signal that instructs immune cells to leave the transplants alone
- Three-month survival confirmed – the modified cells continued producing insulin even as unedited donor cells were destroyed
- No immunosuppressive drugs required – breaking the decades-long requirement for life-limiting anti-rejection medication
- 15-year EU monitoring mandated – ensuring long-term safety and effectiveness tracking
“We transplanted 7% of a curing dose,” explains Per-Ola Carlsson from Uppsala University, acknowledging both the promise and current limitations of this approach.
Reality Check: Progress, Not Perfection
Current limitations point toward the next breakthrough needed for widespread treatment.
Before you cancel your endocrinologist appointments, understand what this breakthrough actually delivers. The patient didn’t achieve complete insulin independence—think of this as proof of concept rather than finished product. The modified cells produced insulin, but not enough to eliminate synthetic insulin entirely.
The real game-changer comes next: replacing limited donor cells with laboratory-grown stem cell-derived insulin producers. This shift would solve the chronic shortage problem while maintaining the immune-evasion advantages, potentially creating an unlimited supply of transplantable cells for the millions managing type 1 diabetes worldwide.
Your current insulin routine—with its daily management demands—represents exactly the kind of chronic treatment model this technology could disrupt. While we’re not there yet, this breakthrough moves diabetes treatment from “lifelong management” toward “functional cure” territory for the first time with genuine scientific backing rather than biotech wishful thinking.
The 15-year monitoring period will reveal whether these engineered cells maintain their insulin production long-term, but for now, your immune system’s ability to coexist with foreign insulin-producing cells has been proven in this specific case.
Last modified: August 9, 2025







